Osteoarthritis of the hip joint is a complex pathology that can cause dangerous consequences for health.
In order to slow down its development and fight dangerous symptoms, it is necessary to consult a doctor in time. The specialist will make the correct diagnosis and choose the appropriate treatment.
Clinical picture and classification of pathology

The pathology is progressive and is accompanied by the destruction of the bones and cartilage of the hip joint. In medicine, this disorder is often called coxarthrosis. It is classified in ICD-10 under code M16.
Most often, the pathology occurs in people over 40 years of age, and women are more susceptible to it.
In elderly people, the disease is associated with the natural aging of the body. The reason for the development of the disease in young people can be traumatic injuries, excess weight, increased physical activity.
In the initial stage of the disease, there are periodic pains in the joint area. Without adequate therapy, the disease progresses, which can lead to disability.
Causes and precipitating factors
The pathology develops gradually and is associated with various factors. The following factors cause the appearance of the disease:
- Hormonal imbalance - can be age or pathological.
- Disruption of blood flow - occurs as a result of injuries, increased physical strength, vascular pathologies.
- Inflammation - can be observed with arthritis.
- Excess weight - increased loads on the hip joint cause its compression and destruction.
- Genetic predisposition - disorders in the structure of the femoral head often cause arthrosis.
- Increased physical activity - rarely provokes arthrosis, but can accelerate the onset of the disease with other negative factors.
- Traumatic injuries - these include sprains, fractures, dislocations.
Stages and types of arthrosis

There are several stages of the development of pathology:
- The first stage - in this stage, uncomfortable feelings appear from time to time. Provocative factor is long-term physical activity. After a short rest, the anxiety subsides.
- The second stage - the pain in the hip joint increases, the groin and thigh are affected. Anxiety also occurs during rest. After a long movement, lameness appears. At this stage, the function of the joint suffers, its motor activity decreases. Contractures develop gradually, strength and muscle mass decrease.
- The third stage - the pain syndrome is permanent and appears even at night. It is very difficult to walk without a cane. Movements are impaired and sharply limited, there is hypotrophy of the muscles of the hip, thigh and lower leg. When moving, a person should lean on the injured side, leaning on the toes.
- The fourth stage - at this stage, the hip joint completely loses motor activity.
Symptoms and manifestations
With the development of this type of arthrosis, the following manifestations occur:
- Severe pain in the affected joint and knee area. Also, groin discomfort may occur. Pain is always present. As the disease worsens, it affects the legs.
- Violation of motor activity. Excruciating pain syndrome impairs a person's ability to move. In this case, he should use a cane or a crutch.
- Shortening of the affected limb.
- Lameness.
- A crisis in the joint that appears with any movement.
- Stiffness of movements.
- Atrophy of muscle tissue in the thigh area is determined by X-rays.
Diagnostic methods of the hip joint

When making a diagnosis, the doctor takes into account the clinical manifestations of the pathology, the anamnesis, the results of the patient's external examination and instrumental studies.
To make an accurate diagnosis, conduct the following studies:
- Analysis of patient complaints and external examination of the damaged area.
- X-ray - with its help, the size of the joint cavity, bone growth, etc.
- Ultrasound procedure.
- Blood tests.
- Magnetic resonance imaging.
If necessary, the inner surface of the articulation is checked using arthroscopic instruments. Differential diagnosis is performed to exclude gonarthrosis, lumbosacral or thoracic osteochondrosis. Pain in arthrosis can be masked as clinical manifestations of radicular syndrome caused by nerve compression or inflammation. It is usually possible to rule out neurogenic pathology with the help of a series of tests. Arthrosis of the hip joint definitely differs from trochanteric bursitis of the hip joint, Bechterew's disease, reactive arthritis. Biochemical studies of blood and synovial fluid are performed to rule out autoimmune pathologies.
Treatment
To cope with arthrosis of the hip joint, it is necessary to choose joint therapy.
General recommendations for daily routine and nutrition
In the initial stage of the pathology, the doctor advises to make lifestyle changes. This will help stop the pain and stop the progression of the disease. At this stage, it is usually enough to adjust the lifestyle and follow a special diet.
The doctor advises the patient to do special physical exercises. Equally important is the correction of the diet. If you are overweight, you must lose weight. Increased joint stress will not allow to eliminate arthrosis.
The basis of the diet should be fish. You can also eat lean meat, legumes, green vegetables, whole grain bread. At the same time, it is recommended to avoid fried foods and fast food. It is necessary to eat sharp, small portions.
Conservative therapy

Medical treatment is aimed at solving such problems:
- pain relief;
- normalization of tissue nutrition;
- stimulation of the regeneration process;
- improved blood flow;
- reducing pressure in damaged areas;
- expansion of the joint space.
To solve these problems, you should use the following categories of drugs:
- Non-steroidal anti-inflammatory drugs. These drugs relieve pain and inflammation. However, they cannot restore the affected cartilage.
- Chondroprotectors. They provide nutrients to the tissues and stop the destruction of the joints, which helps to restore their functions.
- Muscle relaxants. With the help of such means, it is possible to eliminate spasms of muscle tissues and normalize blood flow in tissues.
- Creams and ointments. Such funds activate blood flow and relieve spasms.
- Steroid hormones. These drugs are injected into the joint cavity. Thanks to this, it is possible to cope with the exacerbation of the disease and relieve severe pain.
- Vasodilators. They help the expansion of blood vessels in the joints and provide the tissues with useful substances.
Folk and alternative means
In addition to standard therapy, you can use the following means:
- Tinctures and decoctions for internal use. The basis of such funds can be lemon, mummy, honey, medicinal plants.
- Ointments from natural ingredients. You can use eucalyptus oil, aloe, celandine for their preparation.
- Baths and compresses. Compresses based on cabbage leaves and baths using Jerusalem artichoke can be used to stop the symptoms of arthrosis.
Physiotherapy

In the phase of remission, physiotherapy is actively used:
- Shock wave therapy - in this case, the body is affected by sound waves, which ensures blood flow to any area. It improves the process of regeneration of the dermis and stimulates metabolic processes.
- Myostimulation - helps to restore the activity of muscle tissue weakened due to the forced reduction of motor activity.
- Phonophoresis - a special medicine in the form of an ointment or cream is injected into the affected area under the influence of a special device.
- Ozone therapy - reduces anxiety and activates cartilage development. This effect is achieved as a result of the ozone-oxygen content.
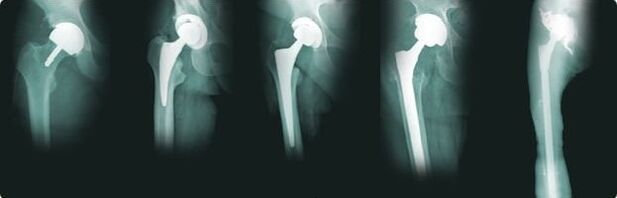
Surgical methods

With the ineffectiveness of conservative therapy, surgical procedures are prescribed:
- Puncture is the removal of excess fluid from the joint. Thanks to this, it is possible to stop pain and normalize physical activity.
- Arthroscopic debridement - includes cleaning the inner joint surface from cartilage elements and washing the cavity with a special solution.
- Periarticular osteotomy is an artificial fracture of the femur. After that, it is closed at a different angle, which minimizes the load on the joint.
- Endoprostheses - in this case, the entire joint is replaced with a prosthesis.
It is impossible to restore the cartilage tissue in a joint damaged by arthrosis without prosthetic surgery, but with the right approach to treatment, following all medical instructions, maintaining the right lifestyle, doing therapeutic exercises, regular massage courses, taking vitamins and proper nutrition, damage to cartilage and hip joints can be prevented. and you can stop the destruction process.
Orthopedic goods
A cane can be used to relieve stress on the hip joint. In some cases, a person is advised to use crutches.
People with this diagnosis are often advised to wear a soft bandage. The use of an orthosis helps reduce the load on the affected area, protects it from dislocations and reduces physical activity.
Effects
In the most difficult situation, a person becomes disabled, completely loses his ability to work and cannot lead an active lifestyle. This situation is very dangerous for the elderly. If you do not help a person, his life is significantly reduced.
Forecast
The pathology has a favorable prognosis for life. In addition, the disease usually progresses slowly. However, there is a risk of life-threatening aseptic necrosis of the femur in some cases.
Arthrosis of the hip joint is a serious pathology that can cause complete loss of motor activity. To prevent this, you should see a doctor on time and strictly follow his recommendations.



















